Case Study
Presented by Martin Cohen, MD
and Robert Princenthal, MD Co-Directors of RadNet’s Prostate Program
PATIENT HISTORY: 65 year old male with elevated PSA, 7.6
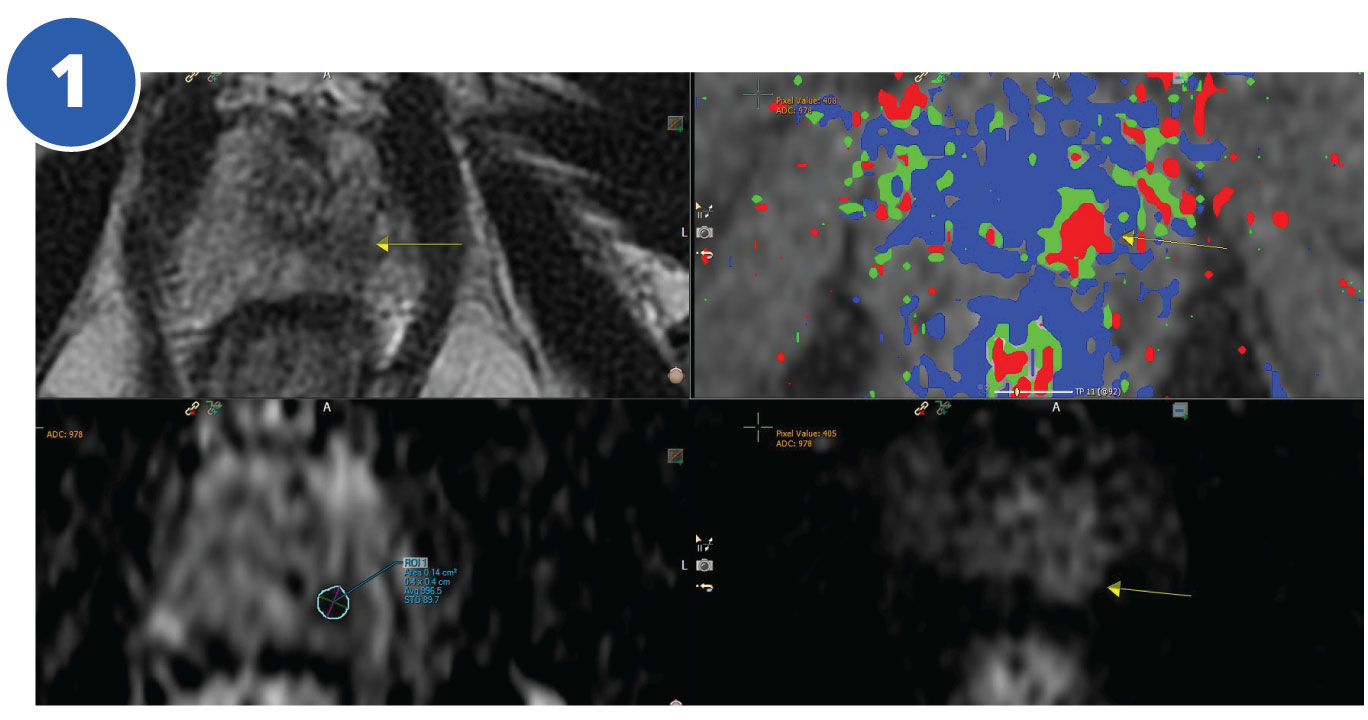
Multiparametric MRI demonstrated a 1.0 CM hypointense nodule left apex (Fig. 1 top left). Low signal on the ADC map-restricted diffusion (bottom left). Increased perfusion (Fig. 1 top & bottom right).
Biopsy performed by the urologist showed Gleason 3+4 left apex 30% core. Additional Gleason 3+3 carcinoma left mid gland and left base 15% core and left apex 5% core.
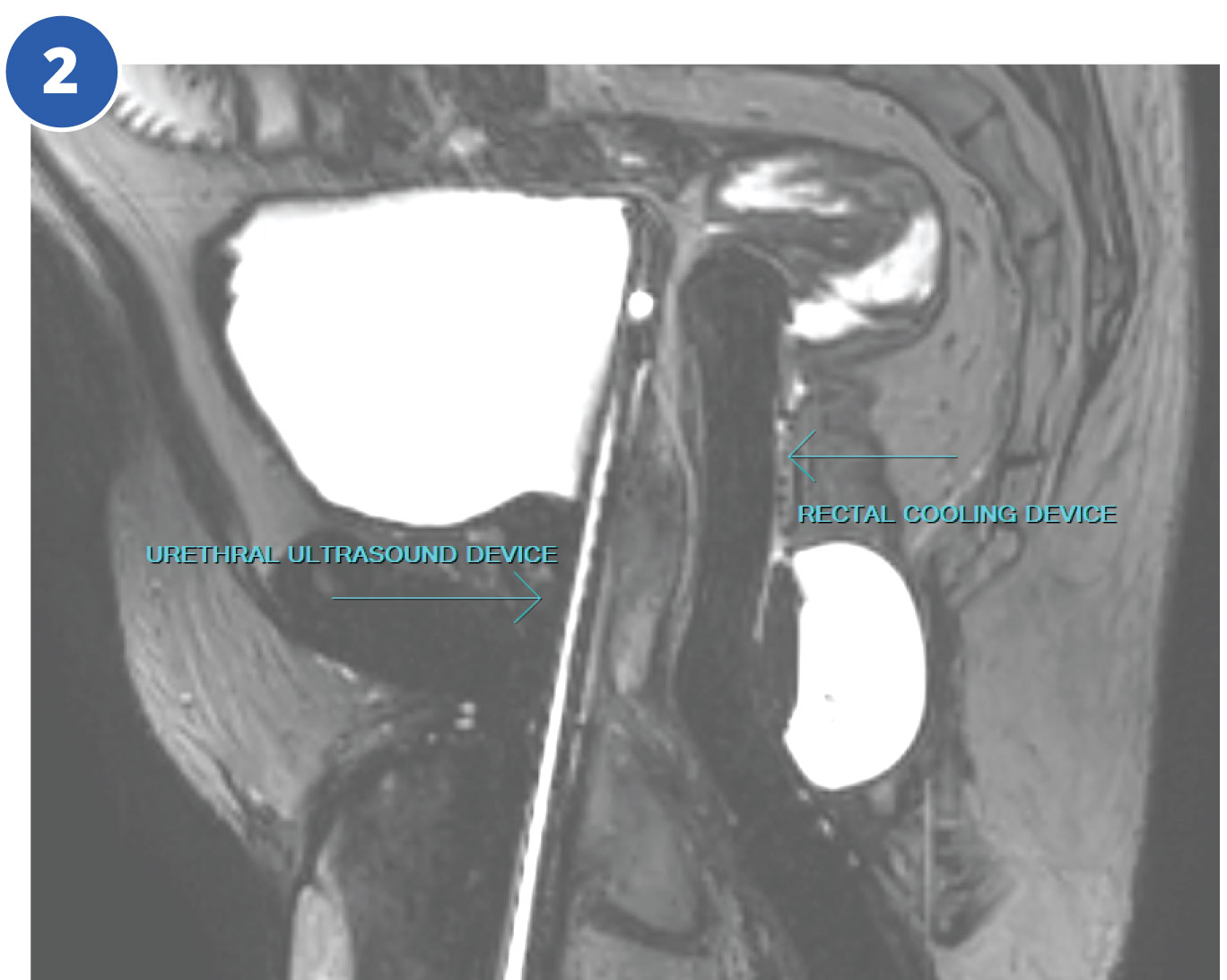
The patient elected to undergo whole gland TULSA ablation as an alternative to radiation therapy or radical prostatectomy. A disposable rotating urethral ultrasound device with 10 treating elements is placed by the urologist. A rectal cooling device is also inserted to protect the rectum from heating (fig.2 – sagittal).
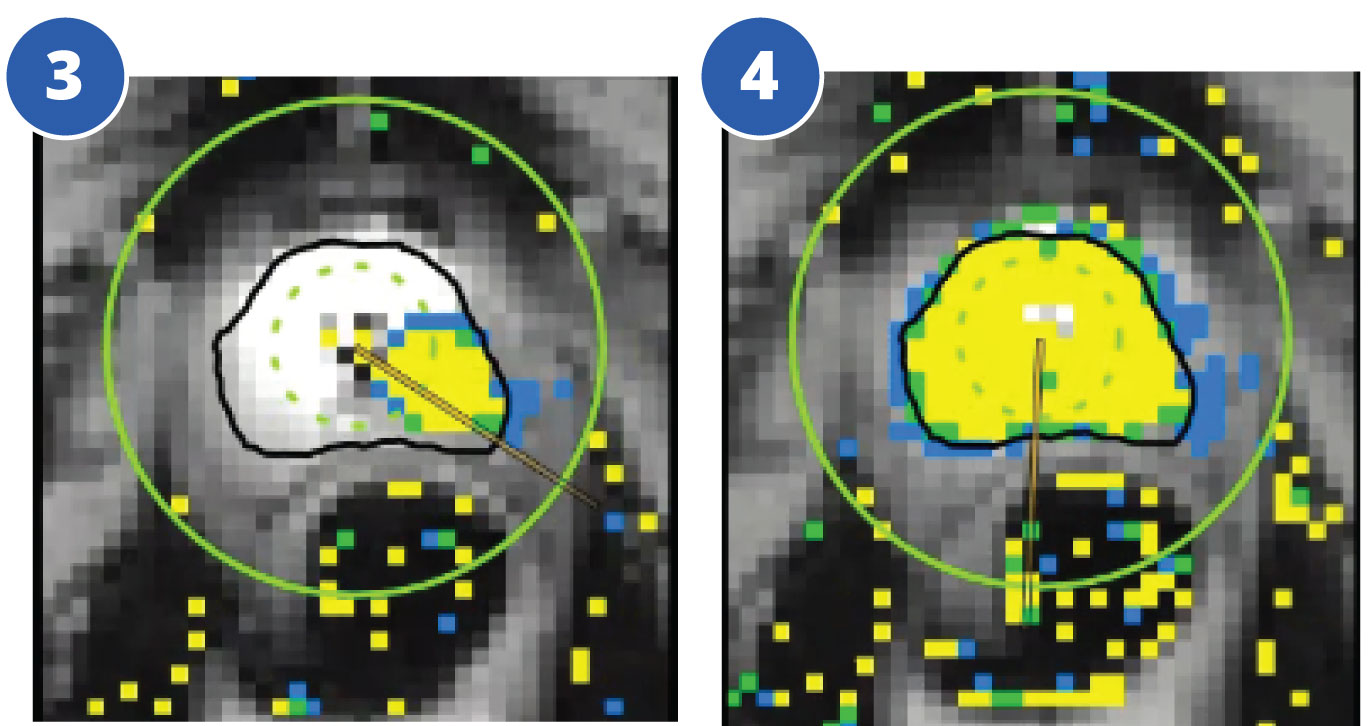
The treatment plan is outlined by the radiologist to preserve the neurovascular bundles and urethral sphincter. During the TULSA procedure the radiologist continuously monitors gland temperature using MRI thermometry. Optimal temperature for irreversible tissue ablation is 55°C (yellow).
- Fig. 3 shows initial treatment in progress (axial)
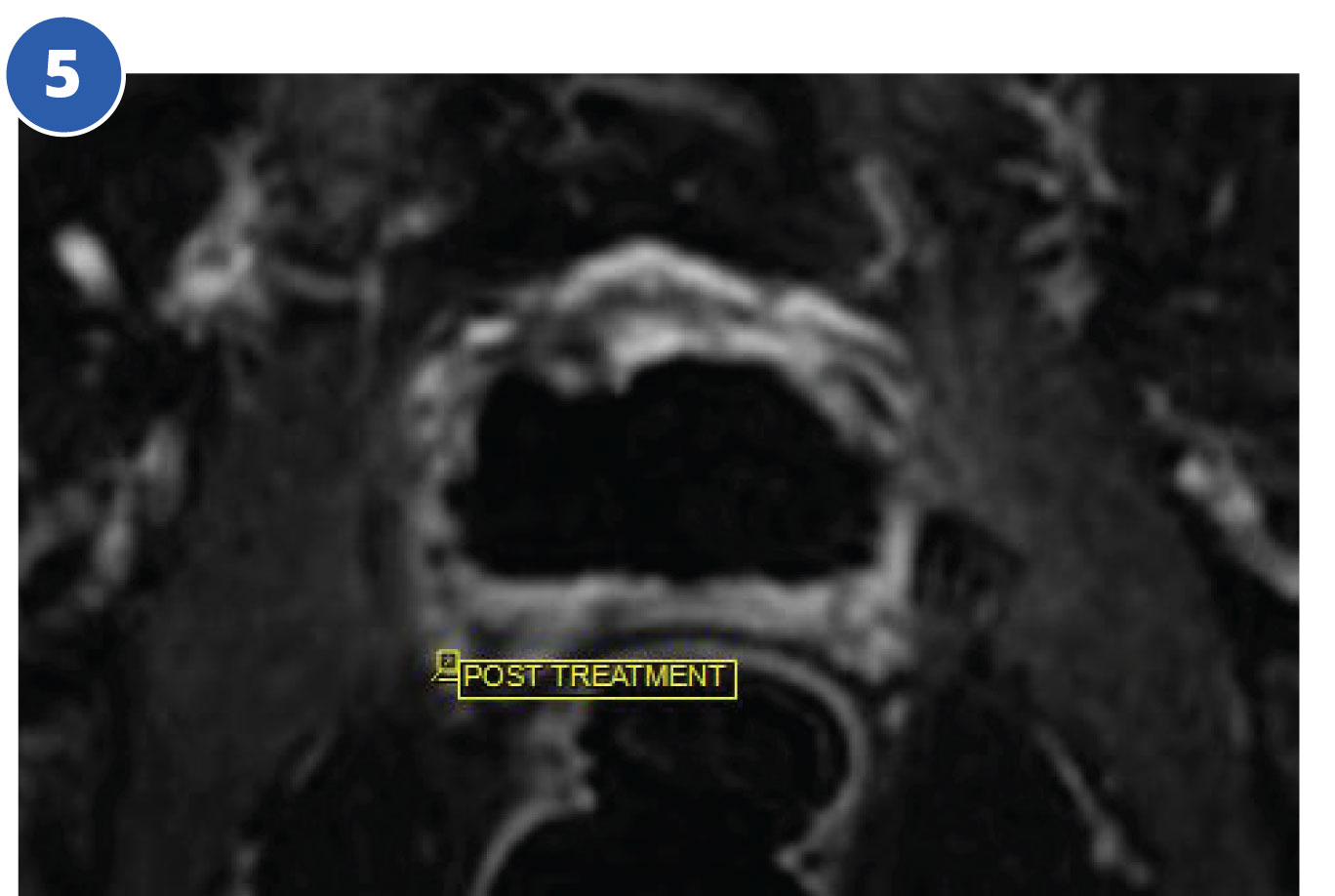
- Fig. 4 following the entire gland treatment (lower midgland level)
- Fig. 5 shows lack of perfusion in the ablated zone following intravenous contrast enhancement.
Following recovery from general anesthesia, the patient is sent home with a Foley catheter for 7 to 10 days.
We Want To Hear From You
Thank you for your interest in RadNet. Please let us know how we can connect with you.
Tulsa Procedure Phone: (818) 480-7266
Tulsa Procedure Fax: (818) 827-5152